Acute Upper Respiratory Tract Infections (Urtis)
Acute upper respiratory tract infections (UTRIs) are predominantly viral in nature. They represent the most common respiratory complaint accounting for 9% of all family practice consultations in the United Kingdom and are the most common category of infectious disease in the United States. The majority of URTIs are mild and self-limiting but a small number give rise to more serious problems, most notably acute epiglottis (a medical emergency) in children and influenza A in elderly patients debilitated by other illnesses. Although viruses are the most common pathogens implicated, the physician must be alert to the possibility of primary bacterial pathogens or perhaps bacterial super-infection following an initial viral illness. High fever, prominent constitutional symptoms, or a prolonged illness are important pointers toward a bacterial etiology necessitating antimicrobial therapy. Some common URTIs are described in the following paragraphs.
Acute Coryza (Common Cold)
The common cold is a symptom complex characterized by nasal congestion, sneezing, rhinorrhoea, pharyngitis, and cough. Over 200 different viral agents including coronaviruses, respiratory syncytial viruses, parainfluenza, and influenza viruses are known to cause coryza although rhinovirus is the most common etiological agent. Transmission is by hand–nose–hand inoculation or by droplet spread; the incubation period is typically 48 to 72 hours. The illness may last for up to 1 week but in up to 25% of patients, it persists for 2 weeks. Immunity is short-lived and virus-specific; most adults will suffer between 2 and 4 coryzal illnesses annually. Children tend to have more frequent colds (6–8 per year) and cigarette smokers also have more frequent viral URTIs. Physical findings are generally confined to the upper respiratory tract and include nasal mucosal edema and pharyngeal erythema. Therapy is principally supportive and includes bed rest, paracetamol (0.5–1 g, 4–6 hourly) for systemic symptoms and fever and nasal decongestants in some cases. The benefits of vitamin C therapy remain unproven (Douglas et al., 2004; Sasazuki et al., 2006). Similarly, data supporting the wide use of the plant extract, echinacea, in coryza are lacking (Linde et al., 2006). Complications of coryza are predominantly due to secondary bacterial infections such as sinusitis (0.5% of cases), otitis media (2% of cases), bronchitis, and pneumonia.
Acute Pharyngitis
Pharyngitis may occur as part of the common cold or as a separate illness. Etiological agents include viruses but also bacteria such as group A beta hemolytic streptococci, Mycoplasma pneumoniae, and Chlamydiae pneumoniae. The patient presents with sore throat and there is erythema of the pharynx often accompanied by tonsillar enlargement. Epstein-Barr virus often affects the pharynx in infectious mononucleosis and there may be associated lymphadenopathy and splenomegaly. A blood film demonstrates atypical monocytes with positive heterophile antibody testing. Streptococcal pharyngitis may be complicated by glomerulonephritis or (rarely) rheumatic fever. With recent advancements in rapid streptococcal antigen testing, throat culture can be reserved for patients in whom symptoms do not improve over time or who do not respond to antibiotics (Vincent et al., 2004). Antibiotic treatment with oral penicillin may reduce the duration of illness and prevent suppurative complications such as pharyngeal abscess.
Acute Sinusitis
Infection of the sinuses causes nasal congestion, purulent nasal discharge, maxillary tooth discomfort, hyposmia, and facial pain or pressure that is worse when bending forward. A variety of organisms may cause acute sinusitis including viruses. In adults Haemophilus influenza, Morexalla catarrhalis, and Streptococcus pneumonia account for 80% of acute bacterial sinusitis. Anaerobic bacteria are also implicated. Acute sinusitis is generally treated with 10–14 days of oral antimicrobial therapy with adjunctive treatments in the form of nasal decongestants and simple analgesia. Therapy should be based on knowledge of local patterns of antibiotic resistance, spectrum of activity against the most common pathogens (including those that are resistant to penicillins and macrolides), and pharmacodynamic potency (Benninger et al., 2006). Complications of acute sinusitis include facial cellulitis, osteomyelitis, intracranial abscess formation, meningitis, and cavernous sinus thrombosis.
Acute Epiglottitis
Acute swelling and inflammation of the epiglottis and aryepiglottic folds is a life-threatening condition usually caused by virulent strains of Haemophilus influenza type B. Death may occur from upper airway occlusion and asphyxiation. It is most common in children aged 2–3 years but can also occur in adults. The illness usually starts with fever and sore throat progressing rapidly with voice changes, drooling, stridor, and respiratory distress. The presence of stridor, voice muffling, rapid clinical course, and underlying diabetes mellitus have been shown to correlate with the need for airway intervention (Katori and Tsukuda, 2005). Direct visualization of the epiglottis may reveal an edematous, erythematous epiglottis projecting over the back of the tongue. Laryngoscopic blade examination should be avoided because of the risk of precipitating total airway obstruction. A lateral cervical X-ray may show epiglottic swelling (thumbprint sign). Blood cultures followed by prompt antibiotic therapy with ampicillin and chloramphenicol, or a thirdgeneration cephalosporin and skilled invasive airway management, are the cornerstones of treatment. Orotracheal or nasal tracheal intubation is usually done under general anesthesia proceeding to tracheostomy if tracheal intubation is not possible. The role of corticosteroids in the management of acute epiglottitis has not been established.
Croup
Croup (acute laryngotracheobronchitis) is usually caused by viruses such as respiratory syncytial virus, influenza A and B, rhinoviruses, adenovirus, and measles. It commonly occurs between 3 months and 3 years of age with a peak incidence in the second year of life. Patients usually present with a barking cough and dyspnea following an upper respiratory tract infection. Supportive treatment with inhalation of steam is widely used despite little evidence (Scolnik et al., 2006). Systemic corticosteroids have reduced the severity of croup, dramatically reduced the need for endotracheal intubation, reduced the need for hospital admission and subsequent length of hospital stay, and reduced the duration of illness (Fitzgerald, 2006).
Influenza
Influenza is an acute systemic viral illness characterized by pyrexia, malaise, myalgia, headache, nasal congestion, and harsh unproductive cough, which may last for several days. It is caused by a group of RNA myxoviruses (commonly types A and B) that are capable of undergoing frequent spontaneous changes in their hemagglutinin and neuraminidase surface antigens referred to as ‘antigenic drift’ if associated with minor outbreaks or ‘antigenic shift’ if associated with epidemics or pandemics. The incubation period is 2 to 4 days and viral spread is via aerosol or mucosal contact with infected secretions. Morbidity and mortality are significant, particularly at extremes of age and in those with underlying cardiorespiratory disease. Viral impairment of mucociliary clearance and macrophage function promotes secondary bacterial infection resulting in pneumonia, bronchitis, or otitis media caused by such organisms as Staphylococcus aureus, Streptococcus peumoniae, and Haemophilus influenzae. Therapy is mainly symptomatic with antipyretics, bed rest, and fluids. Amantadine may ameliorate the symptoms of influenza A if given within the first 24 to 48 h. It may also be used prophylactically in high-risk individuals in epidemics; however, resistance to this agent is emerging (Bright et al., 2005). Annual vaccination is recommended for those with underlying cardiopulmonary disease, renal failure, diabetes, and elderly populations living in nursing homes.
Acute Lower Respiratory Tract Infections (LRTIs)
Acute lower respiratory tract infections (LRTIs) can be divided into those that affect the airways giving rise to bronchitis and those that give rise to pulmonary parenchymal inflammation in the form of pneumonia. As in the upper respiratory tract, both viral and bacterial pathogens are implicated. LRTIs can range in severity from a mild short-lived episode in an otherwise healthy person to a severe life-threatening illness.
Acute Bronchitis
Acute bronchitis is inflammation of the large conducting airways. It is one of the most common diagnoses made by primary care clinicians and emergency department physicians. Cough with or without purulent sputum in association with URTI symptoms suggest the diagnosis of acute bronchitis in an otherwise healthy patient. Bronchitis may present in a manner very similar to pneumonia differing only by the absence of signs of consolidation on chest examination and absent chest X-ray findings. Respiratory viruses appear to be the most common cause of acute bronchitis; however, the organism responsible is rarely identified in clinical practice because viral cultures and serologic assays are not routinely performed. Influenza A and B, coronavirus, rhinovirus, herpes simplex, parainfluenza, and respiratory syncytial virus have all been implicated. Acute bronchitis is a self-limited respiratory disorder, and when the cough persists for more than 3 weeks, other diagnoses must be considered. In the presence of underlying chronic pulmonary disease the manifestations and etiologic agents differ considerably from those seen in the normal host. Bacterial etiologies include H. influenzae, pneumococcus, M. pneumoniae, and B. catarrhalis. B. catarrhalis bronchitis is associated with impaired host defenses and is commonly seen in cigarette smokers or those with preexisting cardiopulmonary disease. Prolonged or high-grade fever is unusual with uncomplicated bronchial infections. Substernal burning or discomfort may be present together with wheeze and rhonci from large airway irritation. Recurrent bouts of acute bronchitis in children should prompt consideration of an underlying immune disorder or respiratory disorder such as cystic fibrosis. Supportive therapy with analgesia, antipyretics, adequate hydration, and assistance with expectoration of viscid secretions may be required. Antimicrobial treatment in acute bronchitis is controversial. The benefits of such treatment have been marginal in many studies, perhaps because of the viral nature of many cases. However, more recent guidelines from the American College of Chest Physicians suggest that widespread use of antibiotics for the treatment of acute bronchitis is not justified, and efforts to curtail their use should be encouraged (Braman, 2006).
Pneumonia
Pneumonia may be defined as inflammation of the substance of the lungs and the term generally implies parenchymal inflammation caused by infection. Globally it is estimated that 5 million children under the age of 5 years die from pneumonia each year (95% in developing countries). There are approximately 4 million cases of community-acquired pneumonia (CAP) annually in the United States, 800 000 of which require hospital admission. Pneumonia is the sixth leading cause of death in the United States and is the most common cause of death from infectious diseases. In the United Kingdom, the incidence is 12 cases per 1000 population per year. About 1 case per 1000 requires hospital admission with approximately 10% of these cases requiring intensive care admission. Admission rates are higher in the elderly (9.62 per 1000 cases). About 25% of all deaths in the elderly are related to pneumonia although this is often the terminal illness in patients with serious concomitant disease. In the outpatient setting, mortality rates for pneumonia remain low, in the range of less than 1–5%. In patients requiring hospitalization, the mortality rate approaches 12% overall, but increases in specific populations such as those with bacteremia and those from nursing home settings. Pneumonia necessitating intensive care admission has a mortality rate approaching 40% overall.
Classification Of Pneumonia
Pneumonia can be classified according to the site affected. It can be localized, affecting just one lobe or segment (lobar), or diffuse, affecting lobules and bronchi and bronchioles (bronchopneumonia). In general terms, lobar pneumonia is seen in previously healthy people while bronchopneumonia is more common in the elderly or those with underlying lung disease. Pneumonia is also classified according to etiology, for example, bacterial, viral, fungal, atypical, chemical, radiation, and allergic.

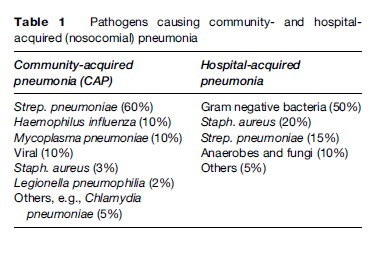
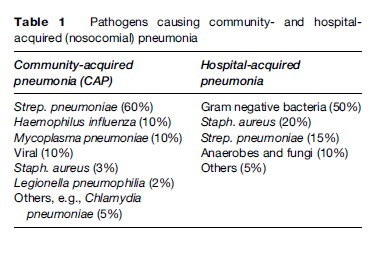
A further classification in widespread clinical use is based on the original source of infection. CAP is defined as acute pulmonary parenchymal infection in a person who has not been hospitalized in the preceding 14 days or is not a resident in a nursing home or long-term care facility. Hospital-acquired (nosocomial) pneumonia is defined as pneumonia occurring 48 hours after hospital admission. It is estimated to occur in 1% of all patients admitted to the hospital and carries a mortality rate approaching 33%. Up to 60% of patients in the intensive care setting develop pneumonia while being ventilated and this form of pneumonia is referred to as ventilator-associated pneumonia (VAP). The spectra of causative organisms in CAP and nosocomial pneumonia are shown in Table 1.
Clinical Features
Patients with pneumonia may present with a constellation of symptoms and signs. Fever or hypothermia is present in about 40–50% of cases. Other symptoms include rigors (15%), pleuritic pain (30%), and new cough with or without purulent sputum (80%). Examination may reveal auscultatory crackles (80%), signs of consolidation (30%), tachypnea (45–70%), and tachycardia (50%). These symptoms and signs may be masked or absent in the elderly.
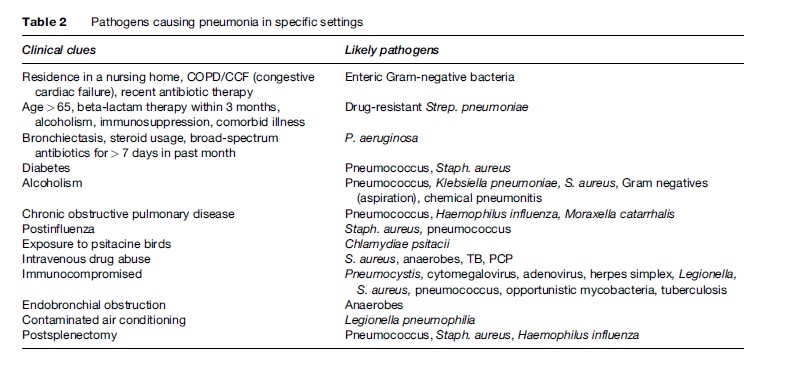
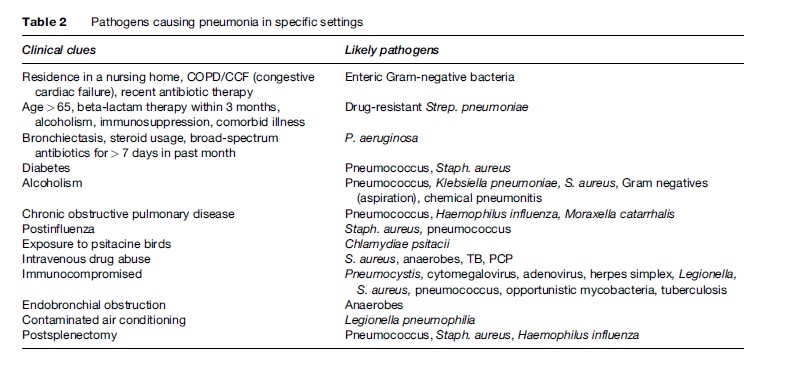
The initial approach to the patient with pneumonia should include an assessment of severity and the need for hospitalization, identification of a likely pathogen, and institution of empiric antibiotic therapy. Specific clues to the likely etiology can often be obtained from history and physical examination and these are summarized in Table 2.
Investigations
Patients with mild pneumonia are usually treated in the outpatient setting and require less investigations than those with more severe pneumonia. The main objectives of investigation in a patient with a clinical diagnosis of pneumonia are to obtain radiological confirmation of the diagnosis, to exclude other conditions that mimic pneumonia, to obtain a microbiological diagnosis, to assess the severity of the pneumonia, and to identify the development of complications. These investigations should include the following:
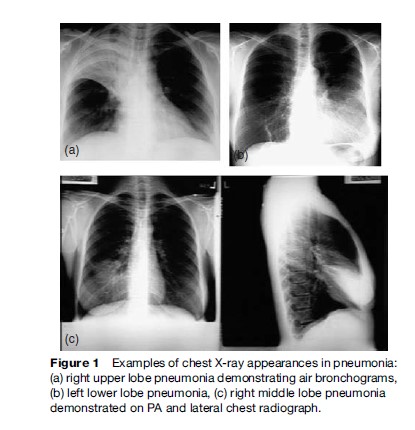
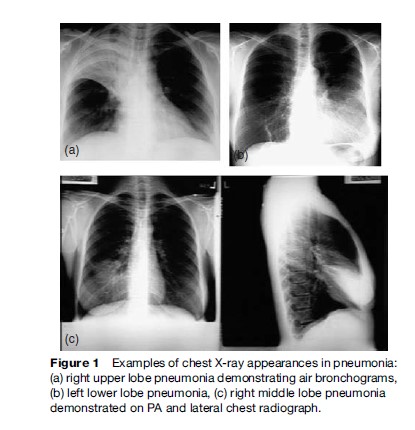
- Chest X-rays confirm the diagnosis by demonstrating areas of consolidation and may help detect complications such as lung abscess or parapneumonic effusion. Examples of chest X-ray changes in pneumonia are shown in Figure 1.
- Sputum Gram stain and culture may help identify a causative organism but prior antibiotic therapy and contamination by oropharyngeal flora may limit their use.
- Blood cultures should be performed in all cases of pneumonia necessitating hospital admission. They are positive in about 30% of cases of pneumococcal pneumonia and in 15% of cases of pneumonia over all.
- Serological testing may allow a retrospective diagnosis of the infecting organism if a rising titer is found between acute and convalescent samples. This is most useful for certain viruses and ‘atypical pneumonia’ organisms such as Mycoplasma pneumoniae.
Severe CAP is considered as pneumonia requiring intensive care unit (ICU) admission. However, no generally accepted definition of severe pneumonia is available and criteria for ICU admission remain undetermined. Each case must be assessed individually. The British Thoracic Society (BTS) criteria for severe pneumonia include two or more of the following clinical signs and laboratory data: hypotension (systolic blood pressure < 90 mmHg, diastolic blood pressure < 60 mmHg), tachypnea (respiratory rate > 30 breaths/min), and confusion or disorientation. Laboratory indices indicative of more severe infection include leukopenia or leukocytosis (WCC < 4000 × 10
9/l or >20 000 ×10
9/l), a raised blood urea (>7 mmol/l), acidosis (pH < 7.35) and hypoxia (PaO
2 < 8 kPa). Other poor prognosticators include age greater than 65, significant comorbidity (e.g., diabetes, congestive cardiac failure [CCF], COPD, immunocompromise, malignancy, chronic renal failure, malnutrition, alcoholism, and cerebrovascular accident). Patients who have been hospitalized within the previous year and those with an extrapulmonary site of infection are also at risk of poorer outcomes. Anemic patients (hemoglobin < 9 gm/dl) and those with evidence of sepsis or organ dysfunction as manifested by metabolic acidosis or coagulopathy have less favorable outcomes.
Figure 1 Examples of chest X-ray appearances in pneumonia: (a) right upper lobe pneumonia demonstrating air bronchograms, (b) left lower lobe pneumonia, (c) right middle lobe pneumonia demonstrated on PA and lateral chest radiograph.
Admission to the ICU is most often because of requirement for mechanical ventilation or inotropic support, either on admission or following failure to improve or clinical deterioration with conventional therapy. The use of noninvasive ventilation, particularly in pneumonia occurring in the COPD population, may support some patients sufficiently to avoid ICU admission. The American Thoracic Society (ATS) guidelines for admission to ICU include either of the following two major criteria: the need for mechanical ventilation or the presence of septic shock; or two out of three of the following minor criteria: multilobar disease, PaO2:FiO2 ratio less than 250, or a systolic blood pressure less than 90 mmHg.
Therapy For Pneumonia
Guidelines from the ATS, European Respiratory Society (ERS), and BTS all recommend empiric treatment for pneumonia based on likely pathogens. All populations should be treated for the possibility of atypical infection with a macrolide alone in the outpatient setting or an intravenous macrolide in hospitalized patients who have no risk factors for drug-resistant Strep. pneumoniae (DRSP), Gram-negatives, or aspiration. Outpatients or non-ICU inpatients with risk factors should be treated with a betalactam and macrolide combination or a fluoroquinolone alone. Both regimens are therapeutically equivalent. In outpatient treatment of the more complicated patient, fluoroquinolone monotherapy may be more convenient than the beta-lactam/macrolide combination. ICU patients should be treated with beta-lactam and macrolide or quinolone using two antipseudomonas agents in at-risk patients.
Conclusion
Acute upper and lower respiratory tract infections are very common causes of morbidity and mortality worldwide. In this chapter, we have reviewed the various clinical presentations, diagnostic approaches, likely etiological agents, and therapeutic considerations for patients who present with acute respiratory tract infections. With the emergence of antimicrobial resistance among many respiratory viral and bacterial pathogens, acute infections of the respiratory tract are likely to continue to pose a significant global health burden in the future. Judicious and appropriate use of antibiotics together with research that improves our understanding of microbial pathogenicity and resistance may help combat such infections and reduce unfavorable outcomes.
Bibliography:
- Benninger MS, Desrosiers M, and Klossek JM (2006) Management of acute bacterial rhinosinusitis: Current issues and future perspectives. International Journal of Clinical Practice 60(2): 190–200.
 Severe CAP is considered as pneumonia requiring intensive care unit (ICU) admission. However, no generally accepted definition of severe pneumonia is available and criteria for ICU admission remain undetermined. Each case must be assessed individually. The British Thoracic Society (BTS) criteria for severe pneumonia include two or more of the following clinical signs and laboratory data: hypotension (systolic blood pressure < 90 mmHg, diastolic blood pressure < 60 mmHg), tachypnea (respiratory rate > 30 breaths/min), and confusion or disorientation. Laboratory indices indicative of more severe infection include leukopenia or leukocytosis (WCC < 4000 × 109/l or >20 000 ×109/l), a raised blood urea (>7 mmol/l), acidosis (pH < 7.35) and hypoxia (PaO2 < 8 kPa). Other poor prognosticators include age greater than 65, significant comorbidity (e.g., diabetes, congestive cardiac failure [CCF], COPD, immunocompromise, malignancy, chronic renal failure, malnutrition, alcoholism, and cerebrovascular accident). Patients who have been hospitalized within the previous year and those with an extrapulmonary site of infection are also at risk of poorer outcomes. Anemic patients (hemoglobin < 9 gm/dl) and those with evidence of sepsis or organ dysfunction as manifested by metabolic acidosis or coagulopathy have less favorable outcomes.
Figure 1 Examples of chest X-ray appearances in pneumonia: (a) right upper lobe pneumonia demonstrating air bronchograms, (b) left lower lobe pneumonia, (c) right middle lobe pneumonia demonstrated on PA and lateral chest radiograph.
Admission to the ICU is most often because of requirement for mechanical ventilation or inotropic support, either on admission or following failure to improve or clinical deterioration with conventional therapy. The use of noninvasive ventilation, particularly in pneumonia occurring in the COPD population, may support some patients sufficiently to avoid ICU admission. The American Thoracic Society (ATS) guidelines for admission to ICU include either of the following two major criteria: the need for mechanical ventilation or the presence of septic shock; or two out of three of the following minor criteria: multilobar disease, PaO2:FiO2 ratio less than 250, or a systolic blood pressure less than 90 mmHg.
Severe CAP is considered as pneumonia requiring intensive care unit (ICU) admission. However, no generally accepted definition of severe pneumonia is available and criteria for ICU admission remain undetermined. Each case must be assessed individually. The British Thoracic Society (BTS) criteria for severe pneumonia include two or more of the following clinical signs and laboratory data: hypotension (systolic blood pressure < 90 mmHg, diastolic blood pressure < 60 mmHg), tachypnea (respiratory rate > 30 breaths/min), and confusion or disorientation. Laboratory indices indicative of more severe infection include leukopenia or leukocytosis (WCC < 4000 × 109/l or >20 000 ×109/l), a raised blood urea (>7 mmol/l), acidosis (pH < 7.35) and hypoxia (PaO2 < 8 kPa). Other poor prognosticators include age greater than 65, significant comorbidity (e.g., diabetes, congestive cardiac failure [CCF], COPD, immunocompromise, malignancy, chronic renal failure, malnutrition, alcoholism, and cerebrovascular accident). Patients who have been hospitalized within the previous year and those with an extrapulmonary site of infection are also at risk of poorer outcomes. Anemic patients (hemoglobin < 9 gm/dl) and those with evidence of sepsis or organ dysfunction as manifested by metabolic acidosis or coagulopathy have less favorable outcomes.
Figure 1 Examples of chest X-ray appearances in pneumonia: (a) right upper lobe pneumonia demonstrating air bronchograms, (b) left lower lobe pneumonia, (c) right middle lobe pneumonia demonstrated on PA and lateral chest radiograph.
Admission to the ICU is most often because of requirement for mechanical ventilation or inotropic support, either on admission or following failure to improve or clinical deterioration with conventional therapy. The use of noninvasive ventilation, particularly in pneumonia occurring in the COPD population, may support some patients sufficiently to avoid ICU admission. The American Thoracic Society (ATS) guidelines for admission to ICU include either of the following two major criteria: the need for mechanical ventilation or the presence of septic shock; or two out of three of the following minor criteria: multilobar disease, PaO2:FiO2 ratio less than 250, or a systolic blood pressure less than 90 mmHg.

